More and more we are hearing about children that have decided that suicide is the only answer for them to escape their sadness or problems they face. Often, I wonder did anyone notice them giving up, isolating, decrease in self-care or no longer reaching out? Unfortunately, in most cases all of these things are not even thought of until after the person is gone. How many times have you read or seen a story in the news where the family, friends and teachers of the person say “ They changed or they didn’t want to do anything” some are able to still smile and pretend they are happy. Some still participate in sports, get good grades and talk about future plans even though they have no desire to be around in those future plans.
Child and adolescent Suicide Awareness will make family, friends and teachers knowledgeable in spotting when their friend or love one is giving up on life. Now that they know how to spot it, what do they do? When looking at the definition of ethics it is described as “what is good for individuals and society, as well as moral philosophy” (BBC, 2014). The BBC (2014) also explains how ethics is about the “other”, meaning that being concerned about someone other than ourselves.
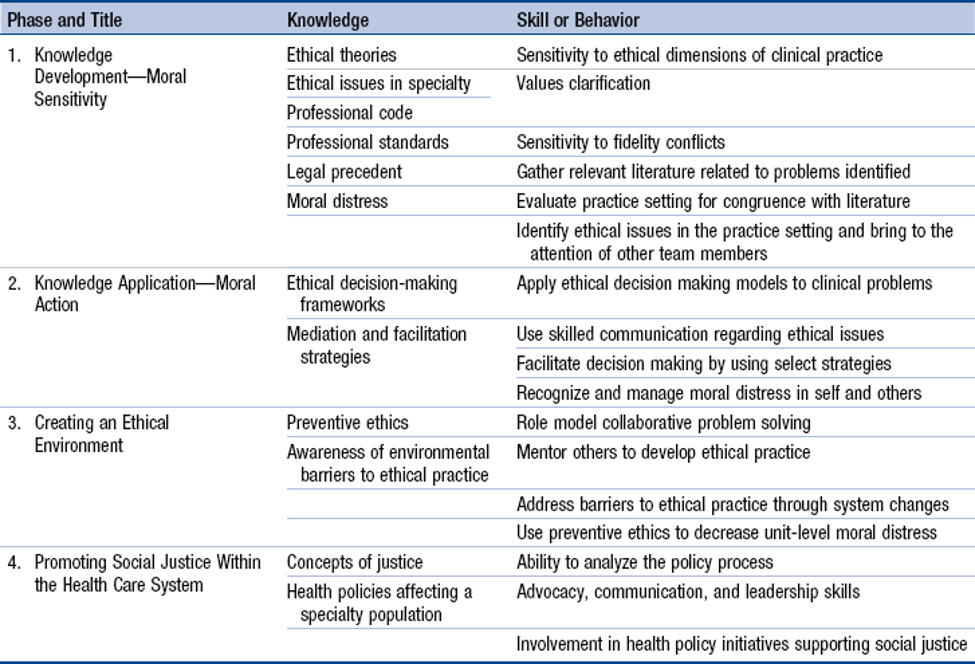
The ethical impact of healthcare policy and the role of ethical decision making in the awareness of child and adolescent suicide is the difference in ending the story for someone or ability of the individual to move on to the next chapter. Healthcare policy incorporates the ethical decision-making model in building healthcare policies that fit all individuals no matter their nationality, sex, age and level of income. Healthcare policies are put in place to improve the public health and have guidelines for all to practice in certain situations that will create consistency in the care of the patients and provide the best outcomes based on evidenced based research. In developing a Healthcare policy starts with an issue or problem that you want to create change for, reviewing and collection data and information on the issues, brainstorming possible solutions, and implementing and monitoring the solution outcomes (Hamric &Delgado, 2016). As you move through the steps to creating the healthcare policy ethical decision-making in applied to all the steps to consider the ethic and legal implications of the change to the problem or issue.
In thinking of the ethical impact and role of ethical decision making in child and adolescent suicidality healthcare policy has pushed to have educators educated on noticing the signs and how to talk to a student about suicide. In the world that we live in it is easy to say “that not my business, or my problem”, when we see someone going through something. But this education of awareness for educator allows them to not only provide a safe environment to talk about these issues with their student but create an open door for students dealing with depression and suicidality.
California has Assembly Bill (AB) 2246, that requires all local education agencies to have suicide prevention policies. AB 2246 mandates that any local education agency servicing students in grades 7-12 create a policy on suicide prevention, intervention, and postvention (California Department of Education, 2019). The policies would include suicide awareness and prevention training for teachers and address the needs of high-risk student groups. The AB 2246 is a health policy that will place some awareness in the schools where youth spend just as much time in as their home.
For the family and friends of those dealing with depression and suicide the National Suicide Prevention Lifeline has the #Bethe1to initiative that provides 5 steps of how to check in on these individuals and provide them with the help they need
Step 1: involves come right out and asking them are they thinking about suicide. Important piece to this is to Never tell them you will keep their suicidal thoughts a secret.
Step 2: Keep them save, this means seeking more information on if they have a plan, what have they already tried and if they have access to the items to complete suicide.
Step 3: Be there for them, this would mean physically, frequent phone calls and texts checking in on them each day. This will create connectedness for them that someone cares about them.
Step 4: Help them connect, this is getting them connected to services and resources of professionals that can help them.
Step 5: Follow up, this means even after they are connected with supports and services that can help them check on them call, visit and text to make sure they are still doing okay. So, we all can change their stories to a happy ending (National Suicide Prevention Lifeline, 2019).

You chose such an important topic that has new meaning and relevance to me lately. One of my dear friends currently has a teenage child battling mental illness. This child has been in and out of the hospital and legal systems as a minor, yet the problem isn’t getting any better. As a last resort, these parents are putting their child through an intensive rehab program, which they will need to pay for out of pocket, as it is not covered by our work insurance. The last time they put their child through a program such as this, they were responsible for over $6000 in psychiatric or medical bills. It is so sad for me to witness this family struggle, as I’m sure many do to provide the best for their children.
In an article by Beck-Little and Catton (2011), the connection between increased hopelessness and suicidal ideation is already evident even in very young children. This gives us a complex challenge as parents and healthcare leaders to address such a serious topic in a uniquely vulnerable population. Physical and sexual abuse were found to lead to suicide attempts in children as young as 3 years old (Beck-Little & Catton, 2011). Thank you for your relevant and impactful post.
Reference
Beck-Little, R., & Catton, G. (2011). Child and Adolescent Suicide in the United States: A Population at Risk. Journal of Emergency Nursing, 37(6), 587-589. doi 10.1016/j.jen.2011.07.018
LikeLiked by 1 person